Incidental Findings Advice for GP & Professionals
The outcome letter provides GPs’ and Professionals’ with advice on actions/considerations needed in light of their patients’ participation in LCS.
Aortic Valve Calcification
The nursing team will screen the patient’s medical history for Aortic Stenosis
GP Advice
Please review findings and offer your patient an appointment to discuss any symptoms.
- If your patient has good exercise tolerance and no symptoms, please refer for a routine local open-access echocardiogram, or cardiology team if this is not available
- If your patient is experiencing exertional symptoms (breathlessness, chest pain or dizziness), please refer for an urgent cardiology outpatient clinic appointment through ERS (Advised from John Morris, Consultant Cardiologist, Liverpool Heart and Chest, Aug 2025)
Emphysema findings on LDCT
GP Advice
Emphysema findings on LDCT
Bone Abnormalities
The nursing team will screen the patient medical history for Osteoporosis, Bone Density Scan in last 12 months, or taking Bisphosphonate medication
GP Advice
Please complete bone risk assessment and prescribe bone protection if required. Consider referral for bone density evaluation
https://cks.nice.org.uk/topics/osteoporosis-prevention-of-fragility-fractures/management/
Bronchiectasis: Moderate and Severe (Asymptomatic at time of LHC)
GP Advice
Please monitor patient for any Bronchiectasis symptoms. If any symptoms of chronic cough or recurrent LRTI please consider referral to the respiratory team.
Coronary Artery Calcification
The nursing team will screen the patients’ medical history for Ischaemic heart Disease, and if they take statin medication.
Advice
History of heart disease and/or takes statin medication
Patient reviewed/managed by Primary Care ie
- Known history of established CVD
- Prescribed lipid lowering medication
- Those that are not new to Lung Cancer Screening Service
In patients not eligible for the CVD prevention service ie those who are not new to LCS, are already prescribed lipid lowering medication or have established CVD the registered practice is advised to refer to https://www.lhch.nhs.uk/lung-health-check for management guidance regarding the finding of coronary artery calcification along with the appropriate Snomed coding to avoid inappropriate inclusion on CVD registers
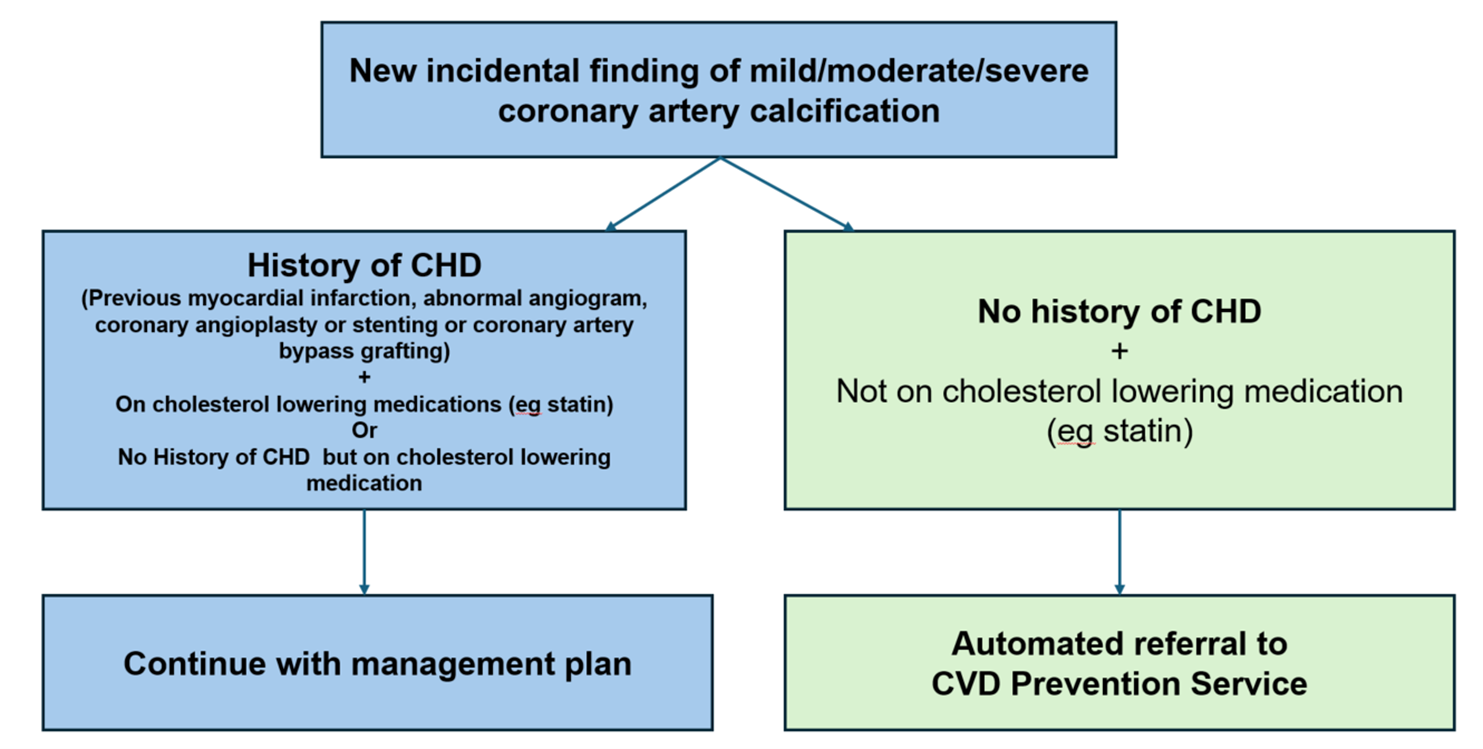
Mild/Moderate/Severe Calcification
Patients who are new to the LCS programme may be eligible for the CVD Prevention Service according to criteria and availability of the service in their area and will be invited to clinic via the LCS team if:
- The patient is NOT prescribed any lipid lowering medication
- The patient DOES NOT have a diagnosis of established CVD
The patient will then be invited to attend the clinic. If they have not been appointed six weeks after their LCS outcome letter the patient may contact the clinic on 0151 600 1005
Please refer to https://www.lhch.nhs.uk/lung-health-check for management guidance for this finding along with the appropriate Snomed coding
Coronary Artery Calcification Primary Care Advisories - August 2025
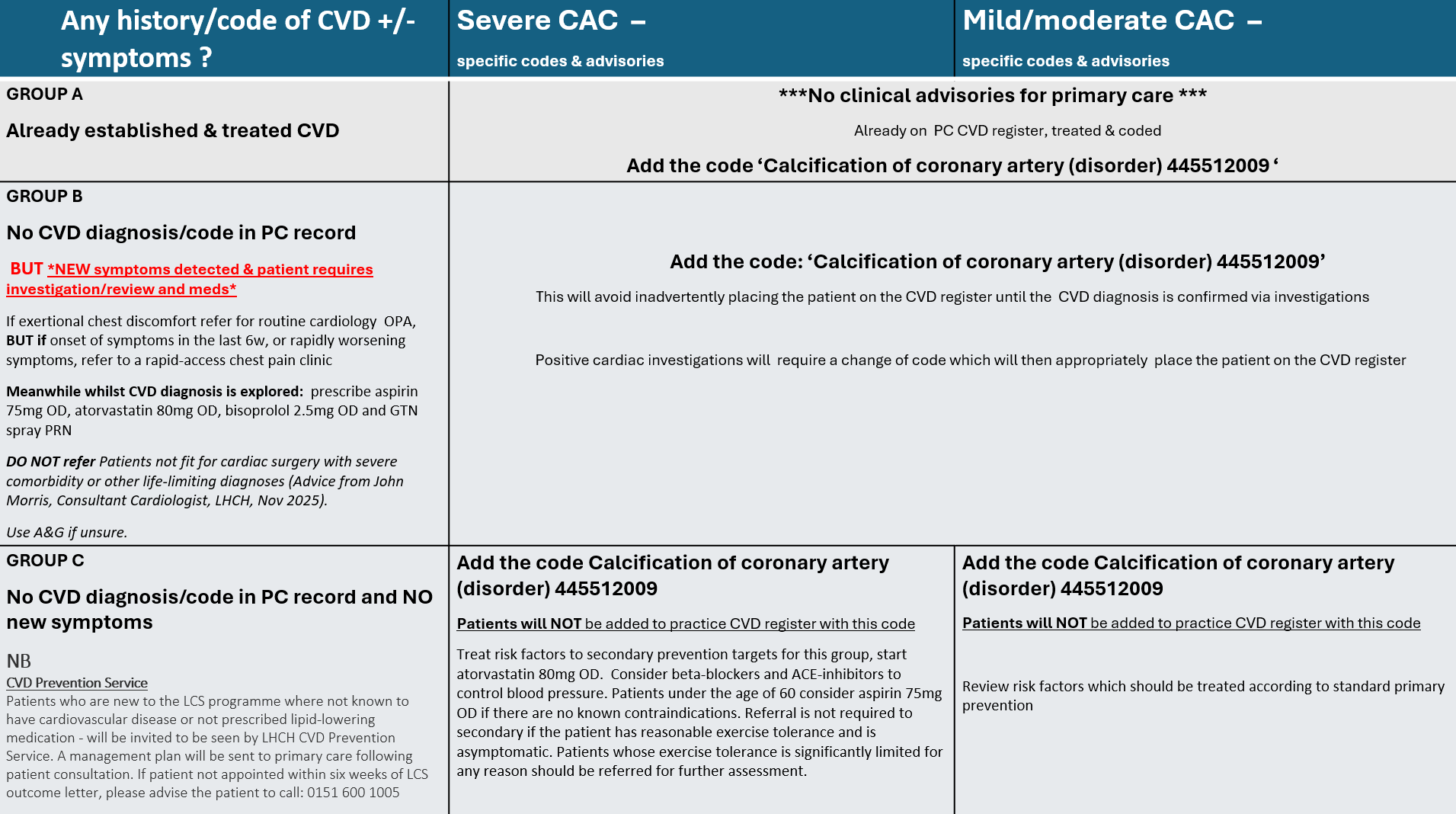
CVD Prevention Service
If patient is not known to have cardiovascular disease and not on cholesterol-lowering medication, they will be invited to be seen by LHCH CVD Prevention Service, and a management plan will be sent to primary care following patient consultation. If patient has not heard anything within two weeks of receiving this letter, then please advise the patient to call: 0151 600 1005.
NB. This service is provided to patients having baseline scans only.
For new findings of Coronary Artery Calcification on interval and follow up scan see advice above.
ACCEPT REFERRAL
✓ Referral received from TLHC - ACCEPT / REJECT
BOOK PATIENT
✓ Order relevant blood tests
CLINICAL ASSESSMENT
✓ Clinical examination
✓ Review new findings
✓ Discuss lifestyle and risk factors
✓ Review medications
✓ Onward referrals (eg smoking cessation, weight management, prediabetics, FH service)
✓ Arrange further investigations (HBPM - diary and equipment, repeat blood tests)
INITIAL STATIN MEDICATION
✓ Dr Morris (LHCH Consultant) to prescribe initial Atorvostatin 20mg to mild/moderate CAC patients
x GPs to prescribe all secondary medications to 'severe CAC' patients
FOLLOW UP REVIEW
✓ Review HBMP results
✓ Review repeat blood tests
✓ Onward referrals (eg GP for hypertension or diabetes diagnosis)
DISCHARGE
✓ Discharge patient back under care of GP
Interstitial Lung abnormalities - 5-10% reticulation without a spirometry result
GP Advice
Lorem ipsum dolor sit amet, consectetur adipisicing elit. Porro labore architecto fuga tempore omnis aliquid, rerum numquam deleniti ipsam earum velit aliquam deserunt, molestiae officiis mollitia accusantium suscipit fugiat esse magnam eaque cumque, iste corrupti magni? Illo dicta saepe, maiores fugit aliquid consequuntur aut, rem ex iusto dolorem molestias obcaecati eveniet vel voluptatibus recusandae illum, voluptatem! Odit est possimus nesciunt.
Please correlate with symptoms of breathlessness and, if symptomatic, consider spirometry testing.
Spirometry showing restriction should be referred to ILD / secondary care clinic for further assessment. GPs to consider utilising Advice & Guidance services for clarity.
Consolidation
GP Advice
In cases where patients have received antibiotics as felt to have infection on CT the GP will need to organise a check CXR at 3m to ensure resolution